Most over-the-counter & prescription sleep aids shouldn't be used for over 2 weeks or in people 65+ due to side effects, falls, confusion, & even dementia. Safer alternatives including melatonin and magnesium can be used to support natural healthy sleep cycles without the same short and long term risks and side effects.
- Insufficient sleep has become a public health epidemic
- Pharmaceutical sleep aids have many risks and can be dangerous
- Natural ingredients including melatonin, magnesium and curcumin promote restful sleep and are a safer alternative to sleep aids
- Practicing good “sleep hygiene” will improve your sleep
- Proprietary Blend SleepHealth uses only natural ingredients with well-established safety and efficacy, even with extended use
Sleep Disorders are A National Epidemic
Insomnia and other sleep disorders are serious problems that are estimated to directly affect 50% of the American population to some extent. Sleep disorders have become such an issue that the Center for Disease Control and Prevention (CDC) has classified insufficient sleep as a public health epidemic. People that do not get adequate sleep are more likely to experience trouble concentrating, memory problems, decreased work productivity, and traffic accidents.2–4 Inadequate sleep can also put you at a higher risk of developing chronic diseases including high blood pressure, Type-2 diabetes, depression, obesity, and cancer.1,2
When you consider all of this and the fact that 50-70 million people have a sleep or wakefulness disorder, it is no surprise that correcting sleep problems is a top priority for the general public and healthcare providers alike. Subsequently, we see a relatively high number of people using over-the-counter (OTC) and/or prescription sleep aids on a fairly regular basis.
What are the risks from using pharmaceutical sleep aids?
Pharmaceutical sleep aids generally fall into a couple different classes. Most of the over-the-counter options rely on the "may cause drowsiness" side-effect common to antihistamines (allergy medicine). Prescription options fall into several different categories including sedative hypnotics, anxiolytics (anti-anxiety), and anti-depressants. All options carry their own unique risks, but some are falling under more scrutiny after recent studies.
Anxiolytics and Sedative Hypnotics
Both classes of prescription sleep aids are known to have high potential for abuse, tolerance, addiction, and falls. They are also known to interfere with a persons mind and this has been a target for new research. A recent study identified a possible link between the use of a class of prescription medications commonly used to treat insomnia and anxiety, called benzodiazepines (BDZ’s), with an increased risk of developing Alzheimer’s disease.5 Sedative hypnotics like zolpidem have similar risk associations plus reports of sleep-walking resulting in injury.
Antihistamine Sleep Aids
Antihistamines are the most commonly used pharmaceuticals found in OTC sleep aids. Antihistamines are typically used for allergies and known for causing drowsiness as a side effect, and that is why they are commonly used as sleep-inducing medications.
Antihistamines belong to a class of medications called “anticholinergics,” that recent research linked to long-term neurological effects. The study, considered to be the largest and most rigorous study of its kind, followed 3,500 participants with an average age of 73 for 7 years and found some alarming results. The researchers looked at the participant’s use of short-term and long-term use of common OTC sleep-aids including Benadryl, Advil PM, Tylenol PM, and Motrin PM (all containing diphenhydramine, an antihistamine, as the active ingredient). They discovered that daily use of these medications for as little as 3 months increased a person’s risk of developing dementia.6
Higher risk with increased use of prescription and OTC sleep aides
The risk of developing dementia appears to be a cumulative dose response, meaning that the longer a person uses a pharmaceutical sleep aid the higher risk they have of developing dementia. The study showed that people using these OTC products daily for 3-7 years had a 54% increased risk of developing dementia compared to only 19% increased risk for those that had used them for 3-12 months.6 It should be noted that current OTC and prescription drug labels recommend not using these types of medications for longer than 2 weeks unless recommended and monitored by your doctor, though people frequently disregard this warning.
Antihistamine Sleep Aides and Alzheimer's Risk
The finding that overuse of antihistamine sleep-aids could possibly increase the risk of conditions like dementia and even Alzheimer's should not come as a complete surprise to most doctors and pharmacists. We have known for several decades that anticholinergic drugs can cause mental disturbances and cognitive impairment, especially in the elderly. In fact, most anticholinergic drugs including common sleep-inducing antihistamines are included on a list of medications that are potentially dangerous or inappropriate for use in people over age 65 for this very reason (see The Beers Criteria).7 We also know that the effects of anticholinergic drugs are tied into Alzheimer’s disease as the most commonly prescribed medication for Alzheimer’s disease [donepezil HCl (Aricept®)] is actually a “cholinergic” drug – meaning it exerts the opposite pharmacological effect of anticholinergic drugs found in OTC sleep aids.
The neurological effects of anticholinergics has been known, but was largely thought to be a temporary short-term reaction, meaning the effects would disappear after stopping the medication. However, this notion was challenged with the most recent data that suggested that the increased risk of dementia persisted even years after discontinuing the medication. This suggests that the neurological effects of anticholinergic medications may be irreversible.6 This significant finding is concerning due to the widespread and frequently long-term unmonitored use of antihistamine-based OTC sleep aids.
Safer Options for Promoting Healthy Sleep
You are not without hope when it comes to finding safe and effective options that are free from the negative side effects seen with the common OTC and prescription sleep aids. There are natural ingredients known to help regulate your sleep cycle and promote restful sleep that have been shown to be a safer alternative for supporting natural sleep including melatonin, magnesium, and curcumin.8–10
Melatonin is produced naturally in your brain when it gets dark, and it helps to regulate your sleep and wake cycles. Your natural melatonin production is highest when you are a child and slowly declines throughout your life, contributing to some of the age-related sleep problems people experience. It has been shown to be a safe and effective option to help maintain a regular sleep cycle. Too much melatonin can actually interfere with your sleep cycles, so it is important to start with a low dose of 1-2 mg before bedtime. If this is not working, you should consult a healthcare provider familiar with sleep disorders and melatonin before increasing your dose. Magnesium and curcumin both provide additional calming and relaxing effects that can help support restful sleep when combined with melatonin.
Practice Good Sleep Hygiene
You should always work to implement non-pharmaceutical methods of improving sleep before turning to pharmaceutical options. Collectively, these methods are referred to as "good sleep hygiene" and they include the following:
- Minimize lights while sleeping. Even small amounts of light can interfere with natural melatonin production. Use a sleep mask if light is unavoidable.
- Get outside into natural lighting during the day.
- Stick to the same bedtime every night.
- Avoid caffeine, nicotine, alcohol, or other chemicals that can interfere with healthy sleep, especially within 8 hours of bedtime.
- Turn down the thermostat while you sleep.
- Don't take your problems to bed. Try to sort out anything weighing on your mind before laying down to sleep.
- Save the bedroom for sleep and intimacy.
- Get adequate physical activity during the day.
- Avoid eating and drinking right before bed as it can contribute to gas, heartburn, and trips to the bathroom that all interrupt sleep.
- Don't go to bed unless your tired.
- Establish a consistent pre-sleep routine to help soothe and calm your mind.
- Use a fan for white noise and to keep good airflow in the room.
- Keep a glass of water next to the bed. If you wake up needing a drink it's best to not have to get out of bed and go to a faucet.
- Limit any daytime naps to 20-30 minutes.
Work With Your Healthcare Providers When Using Stronger Sleep Aids
You need to sleep and there are times when it might be appropriate to include strong OTC or prescription sleep aids, however this is something you should work with your health care providers to determine. Just because a sleep aid is available without a prescription does not mean that it does not contain potent pharmaceutical agents that can cause negative side effects, even years after they have been used.
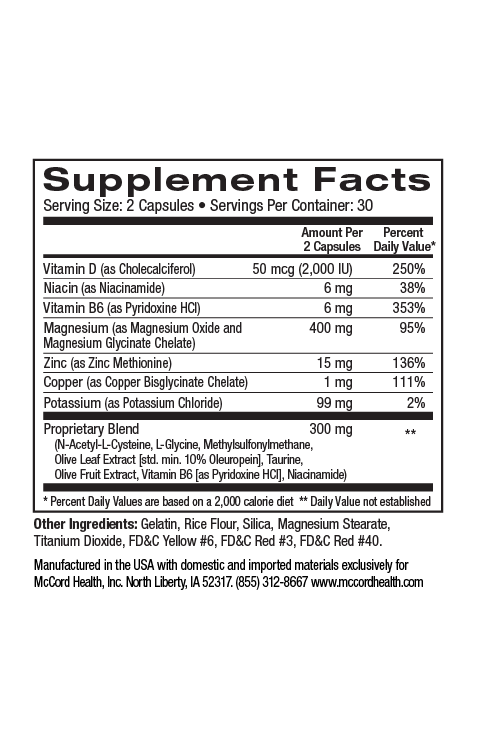
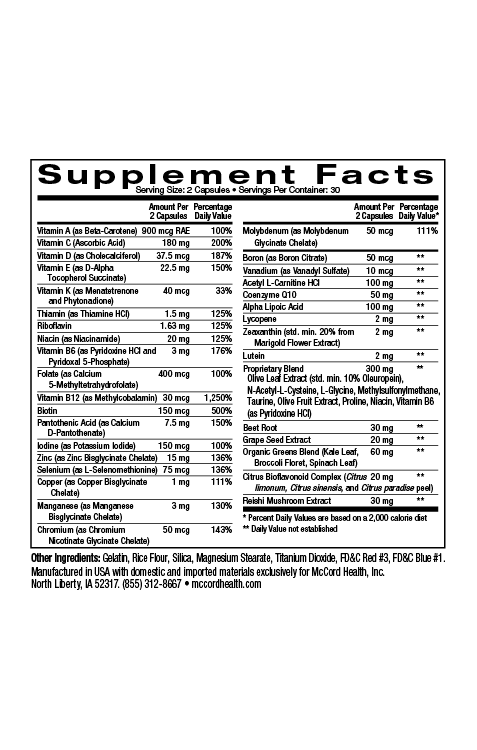
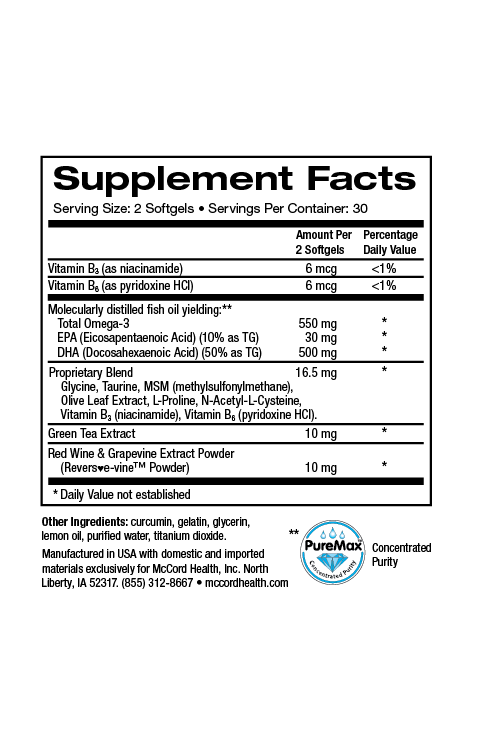
Proprietary Blend SleepHealth only uses natural ingredients with well-established safety and efficacy, even with extended use. If you have been having trouble sleeping and are worried about the long-term effects of OTC or prescription sleep aids, you may benefit from trying Proprietary Blend SleepHealth. You may experience additional benefit by incorporating Proprietary Blend CalmMind. Proprietary Blend EnergyBoost can also be used to help address daytime fatigue and drowsiness.
References
- Centers for Disease Control and Prevention. National Sleep Awareness Week Unhealthy Sleep-Related Behaviors. MMWR. 2011;60(8):1–36.
- Daley M, Morin CM, LeBlanc M, Grégoire J-P, Savard J. The economic burden of insomnia: direct and indirect costs for individuals with insomnia syndrome, insomnia symptoms, and good sleepers. Sleep. 2009;32(1):55–64.
- Spira AP, Kaufmann CN, Kasper JD, et al. Association between insomnia symptoms and functional status in U.S. older adults. J Gerontol B Psychol Sci Soc Sci. 2014;69(7):S35–41.
- Vgontzas AN, Fernandez-mendoza J, Bixler EO, et al. Persistent Insomnia : the Role of Objective Short Sleep Duration and Mental Health. Sleep. 2012;35(1):61–68.
- Billioti de Gage S, Moride Y, Ducruet T, et al. Benzodiazepine use and risk of Alzheimer’s disease: case-control study. BMJ. 2014;349(sep09 2):g5205–g5205.
- Gray SL, Anderson ML, Dublin S, et al. Cumulative Use of Strong Anticholinergic Medications and Incident Dementia. JAMA Intern Med. 2015;175(3):401–7.
- American Geriatrics Society. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4):616–31.
- Zhdanova I V, Wurtman RJ, Regan MM, Taylor J a, Shi JP, Leclair OU. Melatonin treatment for age-related insomnia. J Clin Endocrinol Metab. 2001;86(10):4727–30.
- Abbasi B, Kimiagar M, Sadeghniiat K, Shirazi MM, Hedayati M, Rashidkhani B. The effect of magnesium supplementation on primary insomnia in elderly: A double-blind placebo-controlled clinical trial. J Res Med Sci. 2012;17(12):1161–9.
- Xu Y, Lin D, Li S, et al. Curcumin reverses impaired cognition and neuronal plasticity induced by chronic stress. Neuropharmacology. 2009;57(4):463–71.
- Bastianetto S, Quirion R. Natural Antioxidants and Neurodegenerative Disease. Eur J Clin Nutr. 2004;45:3447–3452.
- Féart C, Samieri C, Rondeau V, et al. Adherence to a Mediterranean diet, cognitive decline, and risk of dementia. JAMA. 2009;302(6):638–48.
- Ogle WO, Speisman RB, Ormerod BK. Potential of Treating Age-Related Depression and Cognitive Decline with Nutraceutical Approaches: A Mini-Review. Gerontology. 2012:1–9.
Disclaimer: These statements have not been reviewed by the FDA. These products are dietary supplements and are not intended to treat, cure, or prevent any disease. The decision to use these products should be discussed with a trusted healthcare provider. The authors and the publisher of this work have made every effort to use sources believed to be reliable to provide information that is accurate and compatible with the standards generally accepted at the time of publication. The authors and the publisher shall not be liable for any special, consequential, or exemplary damages resulting, in whole or in part, from the readers’ use of, or reliance on, the information contained in this article. The publisher has no responsibility for the persistence or accuracy of URLs for external or third party Internet websites referred to in this publication and does not guarantee that any content on such websites is, or will remain, accurate or appropriate.