Most people would agree that nothing really beats a great night of restful sleep. Most cells in your body would also agree that they appreciate a good night’s rest. However, there are certain types of cells that cannot stand it when you get a full night of great sleep – and those are cancer cells.
We know that sleep is important for feeling rested and energetic during the day, improving mood, immunity, work performance, heart health, cognition – more things than can possibly be imagined. But would you believe that the quality and amount of sleep you get could actually change the way your body responds to certain medications? In fact, as in the case of the breast cancer drug tamoxifen, it could be the difference in treatment success or failure.
For over 20 years, studies have shown that the sleep hormone melatonin plays a role in the behavior of various types of cancers including prostate and breast cancer.1 Melatonin is responsible for telling your brain that it is time to sleep, but the research is showing that it can essentially tell cancer cells that they also need to sleep.1–5
It is only during these sleep phases that some anti-cancer drugs like tamoxifen can attack the cancer cells and stop them from multiplying. Several studies have shown that having increased blood levels of melatonin can improve the success of tamoxifen in treating breast cancer.6–8
How Does the Brain Produce Melatonin?
Your brain contains a tiny gland called the pineal gland that wants to constantly produce melatonin. However, when you can see light, there are signals sent to the gland that stop it from producing melatonin. This is what helps regulate your daily sleep cycle, called the “circadian rhythm.”
When you enter a dark room, the pineal gland begins pumping out melatonin, causing you to feel tired and go to sleep. Therefore, it is important to remove yourself from all light-sources when you sleep. Even small amounts of light can cause a decreased production of melatonin resulting in lower quality of sleep.7
Your pineal gland produces the most melatonin early in life, generally peaking around age five. It then steadily produces less and less melatonin as you age, which is one of the reasons that people tend to have more sleep disorders as they get older. This decline in melatonin production may also be responsible for the development of others diseases and cancers associated with age.2–4,9,10
Melatonin and Breast Cancer
Several studies have shown that melatonin has anticancer properties with evidence that it can help inhibit the growth and spread of some cancer cells.1,9–13 The studies that looked at the effect of melatonin concentrations on the efficacy of tamoxifen for breast cancer found that small amounts of light, similar to the amount that would come underneath a closed door or from a nightlight, were actually capable of lowering melatonin levels far enough to decrease the efficacy of the medication.6,8,7
The fact that such low levels of light had such profound effects on melatonin levels and the efficacy of anti-cancer medications should cause alarm for some. In our modern world, it is almost impossible to escape "light pollution" that comes from city lights, televisions, and computer screens.
Many view the findings of the melatonin and tamoxifen studies as compelling evidence to include supplemental melatonin as a standard part of breast cancer medication regimens, especially in those using tamoxifen and those who may be at risk of decreased melatonin production due to age, genetic predisposition, medical conditions, and light pollution.1,9,6,8,7
Supplementing Melatonin
Before you start taking melatonin, there are a couple things you need to know. First, like most medications, taking more does not always mean it will work better and could have negative effects. If you take too large of a dose of melatonin at bedtime, your body may not be able to effectively reduce those levels to what they should be in the morning when you want to be awake and alert, causing a disruption in your circadian rhythm.14
Doses of 2 mg or less, like what is included in Viniferamine Sleep Support have been shown to be safe and effective while providing blood levels that are similar to those found in a natural healthy sleep cycle.14–17 Some people may require more than 2 mg, however that dose should be determined by a licensed healthcare provider that is carefully monitoring the response.
Something else to consider when adding a melatonin supplement is that melatonin does not work alone. In particular, studies have indicated that a potent antioxidant called glutathione is important for the anti-cancer properties observed with melatonin as the effects are diminished when glutathione is removed or depleted.12
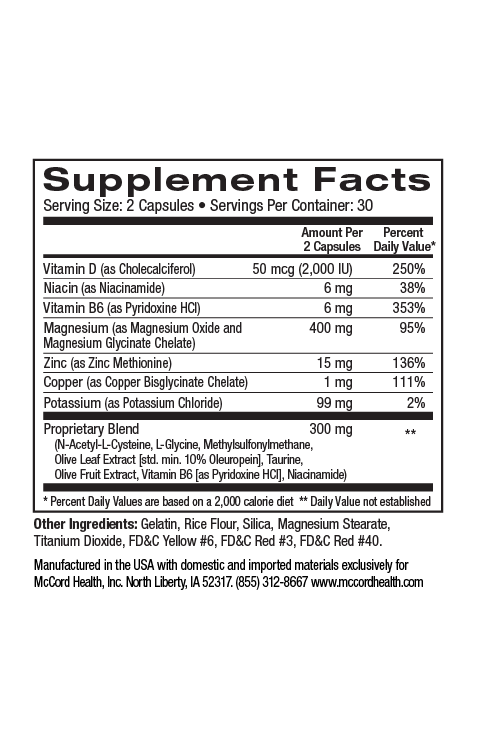
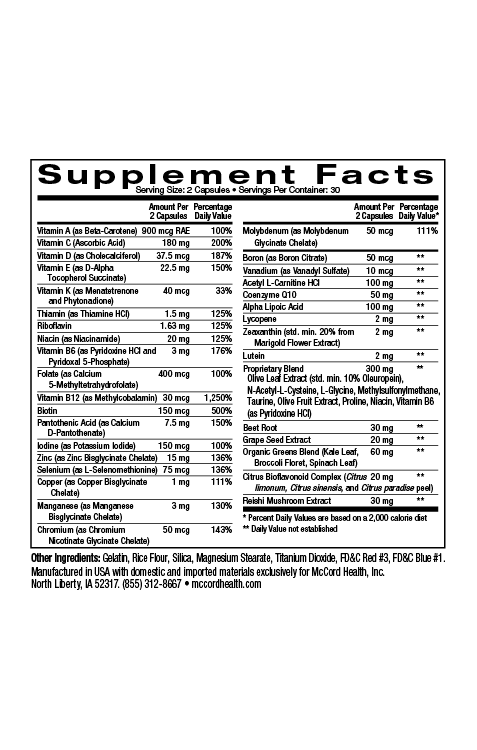
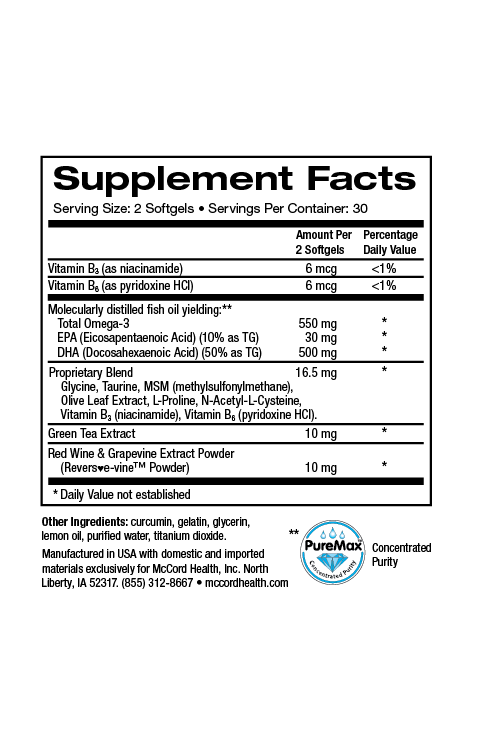
Your body does not absorb glutathione from the diet, but prefers to make its own glutathione from a couple of key building blocks that are more easily absorbed. Viniferamine Sleep Support contains Olivamine10 Max and one of the key components in this blend is N-acetyl-L-cysteine (NAC). NAC is the key nutrient required for increasing cellular levels of glutathione.18,19 All of the ingredients found in Viniferamine Sleep Support combine to help provide your body the nourishment and healing rest that it needs.
References
- Jung B, Ahmad N. Melatonin in cancer management: progress and promise. Cancer Res. 2006;66(20):9789-9793.
- Schernhammer ES, Schulmeister K. Melatonin and cancer risk: does light at night compromise physiologic cancer protection by lowering serum melatonin levels? Br J Cancer. 2004;90(5):941-943.
- Zhdanova I V, Wurtman RJ, Regan MM, Taylor J a, Shi JP, Leclair OU. Melatonin treatment for age-related insomnia. J Clin Endocrinol Metab. 2001;86(10):4727-4730.
- Brzezinski A. Melatonin in humans. N Engl J Med. 1997;336(3):186-195.
- León J, Acuña-Castroviejo D, Escames G, Tan D-X, Reiter RJ. Melatonin mitigates mitochondrial malfunction. J Pineal Res. 2005;38(1):1-9.
- Lissoni P, Barni S, Meregalli S, et al. Modulation of cancer endocrine therapy by melatonin: a phase II study of tamoxifen plus melatonin in metastatic breast cancer patients progressing under tamoxifen alone. Br J Cancer. 1995;71(4):854-856.
- Dauchy RT, Xiang S, Mao L, et al. Circadian and Melatonin Disruption by Exposure to Light at Night Drives Intrinsic Resistance to Tamoxifen Therapy in Breast Cancer. Cancer Res. 2014;74:4099-4110.
- Wilson ST, Blask DE, Lemus-Wilson AM. Melatonin augments the sensitivity of MCF-7 human breast cancer cells to tamoxifen in vitro. J Clin Endocrinol Metab. 1992;75(2):669-670.
- Blask DE, Sauer LA, Dauchy RT. Melatonin as a Chronobiotic / Anticancer Agent: Cellular, Biochemical, and Molecular Mechanisms of Action and their Implications for Circadian-Based Cancer Therapy. Curr Top Med Chem. 2002;2(2):20.
- Moss RW. Should patients undergoing chemotherapy and radiotherapy be prescribed antioxidants? Integr Cancer Ther. 2006;5(1):63-82.
- Cos S, Fernández R, Güézmes A. Influence of Melatonin on Invasive and Metastatic Properties of MCF-7 Human Breast Cancer Cells. Cancer Res. 1998;58:4383-4390.
- Blask DE, Wilson ST, Zalatan F, Blask E. Physiological Melatonin Inhibition of Human Breast Cancer Cell Growth in Vitro : Evidence for a Glutathione-mediated Pathway. Cancer Res. 1997;57:1909-1914.
- Hill SM, Blask DE. Effects of the Pineal Hormone Melatonin on the Proliferation and Morphological Characteristics of Human Breast Cancer Cells ( MCF-7 ) in Culture. Cancer Res. 1988;48:6121-6126.
- van Geijlswijk IM, Korzilius HPLM, Smits MG. The use of exogenous melatonin in delayed sleep phase disorder: a meta-analysis. Sleep. 2010;33(12):1605-1614.
- Lewy AJ. Clinical applications of melatonin in circadian disorders. Dialogues Clin Neurosci. 2003;5(4):399-413.
- Benloucif S, Ph D, Burgess HJ, et al. Measuring Melatonin in Humans. J Clin Sleep Med. 2008;4(1):66-69.
- Burgess HJ, Revell VL, Eastman CI. A three pulse phase response curve to three milligrams of melatonin in humans. J Physiol. 2008;586(2):639-647.
- Nguyen D, Hsu JW, Jahoor F, Sekhar R V. Effect of increasing glutathione with cysteine and glycine supplementation on mitochondrial fuel oxidation, insulin sensitivity, and body composition in older HIV-infected patients. J Clin Endocrinol Metab. 2014;99(1):169-177.
- Atkuri KR, Mantovani JJ, Herzenberg L a, Herzenberg L a. N-Acetylcysteine--a safe antidote for cysteine/glutathione deficiency. Curr Opin Pharmacol. 2007;7(4):355-359.